Inflammation Causes Disease: Cryotherapy Can Help
The article below discusses the adverse effects chronic inflammation can have on our health. There are very few treatments for chronic, systemic inflammation: most involve drug-intervention like NSAIDs Celebrex etc. Whole body cryotherapy is one of the only non-invasive, non-pharmaceutical, safe treatment for reducing systemic chronic inflammation. It is highly effective, efficient (sessions are a maximum of 3 minutes) and safe!!
Dr. David M. Marquis, DC, DACBN
Inflammation controls our lives. Have you or a loved one dealt with pain, obesity, ADD/ADHD, peripheral neuropa‐ thy, diabetes, heart disease, stroke, migraines, thyroid issues, dental issues, or cancer?
If you answered yes to any of these disorders you are dealing with inflammation.
Sadly, most of us are suffering from one or more of these disorders but have no idea how to eliminate inflamma‐ tion. Most doctors are utilizing pharmaceuticals in lieu of getting to the root cause.
It often seems extremely foreign to most people when they realize the majority of inflammatory diseases start in the gut with an autoimmune reaction which progresses into systemic inflammation. To truly be effective at man‐ aging or hopefully overcome a disease it needs to be addressed on all levels. Taking a look at where this process starts is the key.
Where Does Inflammation Begin?
Your gut is made of an incredibly large and intricate semi-permeable lining. The surface area of your gut can cover two tennis courts when stretched out flat.
Its degree of permeability fluctuates in response to a variety of chemically mediated conditions. For example when your cortisol is elevated due to the stress of an argument or your thyroid hormone levels fluctuate due to burning the midnight oil your intestinal lining becomes more permeable in real time.
Then you sit down to eat and partially undigested food, toxins, viruses, yeast, and bacteria have the opportunity to pass through the intestine and access the bloodstream, this is known as leaky gut syndrome, or LGS.
When the intestinal lining is repeatedly damaged due to reoccurring leaky gut syndrome, damaged cells called microvilli become unable to do their job properly. They become unable to process and utilize the nutrients and enzymes that are vital to proper digestion. Eventually, digestion is impaired and absorption of nutrients is negatively affected. As more exposure occurs, your body initiates an attack on these foreign invaders. It responds with inflam‐ mation, allergic reactions, and other symptoms we relate to a variety of diseases.
So you might ask, what’s the harm of inflammation and ongoing allergic reactions?
It may sound relatively harmless, but this situation can and often does lead to numerous serious and debilitating dis‐ eases. Since your immune system can become overburdened, these inflammatory triggers are cycled continuously through your blood where they affect nerves, organs, connective tissues, joints, and muscles. You can probably begin to see how diseases develop.
Inflammation Triggers the Symptoms of Disease
The presence of inflammation is what makes most disease perceptible to an individual. It can and often does occur for years before it exists at levels sufficient to be apparent or clinically significant. How long it has been smoldering really determines the degree of severity of a disease and often the prognosis assuming the inflammation can be con‐ trolled. One could also argue that without inflammation most disease would not even exist. Take a look at this list of diseases and their relationship with inflammation:
Disease Mechanism
- Allergy: 4 Immune Mediated Types + Sensitivities, all of which cause inflammation
- Alzheimer’s: Chronic inflammation destroys brain cells
- Anemia: Inflammatory cytokines attack erythropoietin production
- Ankylosing Spondylitis: Inflammatory cytokines induce autoimmune reactions against joint surfaces
- Asthma: Inflammatory cytokines induce autoimmune reactions against airway lining
- Autism: Inflammatory cytokines induce autoimmune reactions in the brain arresting right hemisphere development
- Arthritis: Inflammatory cytokines destroy joint cartilage and synovial fluid
- Carpal Tunnel Syndrome: Chronic inflammation causes excessive muscle tension shortening tendons in the forearm and wrist compressing the nerves.
- Celiac: Chronic immune mediated inflammation damages intestinal lining
- Crohn’s Disease: Chronic immune mediated inflammation damages intestinal lining
- Congestive heart failure: Chronic inflammation contributes to heart muscle wasting
- Eczema: Chronic inflammation of the gut and liver with poor detoxification and often antibodies against Transglutaminase-3.
Fibromyalgia: Inflamed connective tissue often food allergy related and exacerbated by secondary - nutritional and neurological imbalances.
- Fibrosis: Inflammatory cytokines attack traumatized tissue
- Gall Bladder Disease: Inflammation of the bile duct or excess cholesterol produced in response to gut inflammation
- GERD: Inflammation of the esophagus and digestive tract nearly always food sensitivity and pH driven
- Guillain-Barre: Autoimmune attack of the nervous system often triggered by autoimmune response to external stressors such as vaccinations.
- Hashimoto’s Thyroiditis: Autoimmune reaction originating in the gut triggered by antibodies against thyroid enzymes and proteins
- Heart attack: Chronic inflammation contributes to coronary atherosclerosis
- Kidney failure: Inflammatory cytokines restrict circulation and damage nephrons and tubules in the kidneys
- Lupus: Inflammatory cytokines induce an autoimmune attack against connective tissue
- Multiple Sclerosis: Inflammatory cytokines induce autoimmune reactions against myelin
- Neuropathy: Inflammatory cytokines induce autoimmune reactions against myelin and vascular and connective tissues which irritate nerves.
- Pancreatitis: Inflammatory cytokines induce pancreatic cell injury
- Psoriasis: Chronic inflammation of the gut and liver with poor detoxification
- Polymyalgia Rheumatica: Inflammatory cytokines induce autoimmune reactions against muscles and connective tissue
- Rheumatoid Arthritis : Inflammatory cytokines induce autoimmune reactions against joints
- Scleroderma: Inflammatory cytokines induce an autoimmune attack against connective tissue
- Stroke: Chronic inflammation promoted thromboembolic events
- Surgical complications: Inflammatory cytokines (often pre-dating the surgery) slow or prevent healing
Why Inflammation Must Be Addressed at its Root…
The fact that your immune system drives the inflammatory process in disease is well established. Unfortunately Western medicine offers little in the way of actual answers as to managing or overcoming the Autoimmune process. The typical approach to therapy is generally to suppress the immune response with Immune suppressive agents or sometimes steroids. Both approaches are designed to reduce inflammation but neither stops the underlying disease processes or allows for damaged tissues to regenerate.
Unless you turn off the actual cause of fire (inflammation), all you have done is postponed the inevitable and potentially destroyed more of the building (your body) in the process, by allowing the fire to smolder in a subclinical fashion.
Every day on TV you can see professional athletes and others acting as spokespeople for Methotrexate, Orencia, Enbrel, Humira, Remicade, and other drugs which largely are designed to mask inflammation or suppress the immune response. None of these drugs actually have the capacity to correct the underlying condition and yet the imagery the ads leave the viewer with is that you will have your life back.
The Link Between Gut Dysfunction and Inflammatory Diseases
The term inflammation rarely elicits a truly accurate image in the mind of someone unless they are experiencing it. Then it begins to make sense because of the pain and dysfunction associated with inflammation. The ability to be inflamed is absolutely necessary for normal repair processes to occur. It is when the regulation of inflammation is not tempered or controlled that we begin to have a problem with inflammation.
It has been shown that many of the inflammatory diseases we suffer from are gut mediated but not presenting as gut issues. Dr. Maios Hadjivassiliou of the United Kingdom, a world authority on gluten sensitivity, has reported in The Lancet, that “gluten sensitivity can be primarily and at times, exclusively a neurological disease.” This means that people show gluten sensitivity by having problems with brain function despite having no gastrointestinal problems whatsoever. Dr. Hadjivassiliou indicates that the antibodies that a person has when they are gluten sensitive can be directly and uniquely toxic to the brain. For this there are specialty tests that have been developed.
Another author, published in a recent issue of Pediatrics, stated, “This study suggests that the variability of neurologic disorders that occur in celiac disease is broader than previously reported and includes softer and more common neurologic disorders including chronic headache, developmental delay, hypotonia and learning disorders or ADHD.” Clearly we have to broaden our evaluation criteria and perhaps definition of disease when a patient presents with complaints that do not fit into a typical clinical box.
How to Evaluate Inflammatory Diseases
Since inflammation is commonly mediated by the gut it is a logical starting point in the evaluation process of any patient. There are seven common areas that should be considered when looking at causative factors for gastrointestinal dysfunction that create the environment for chronic inflammation. They are listed below along with key triggers within the category of evaluation:
- Diet: Alcohol, Gluten, Casein, Processed Foods, Sugar, Fast Food
- Medications: Corticosteroids, Antibiotics, Antacids, Xenobiotics
- Infections: Such as H-Pylori, Yeast or Bacterial Overgrowth, Viral or Parasite Infection
- Stress: Increased Cortisol, Increased Catecholamines
- Hormonal: Thyroid, Progesterone, Estradiol, Testosterone
- Neurological: Brain Trauma, Stroke, Neuro-degeneration
- Metabolic: Glycosylated End Products (inflammatory end products of sugar metabolism), Intestinal Inflammation, Autoimmune
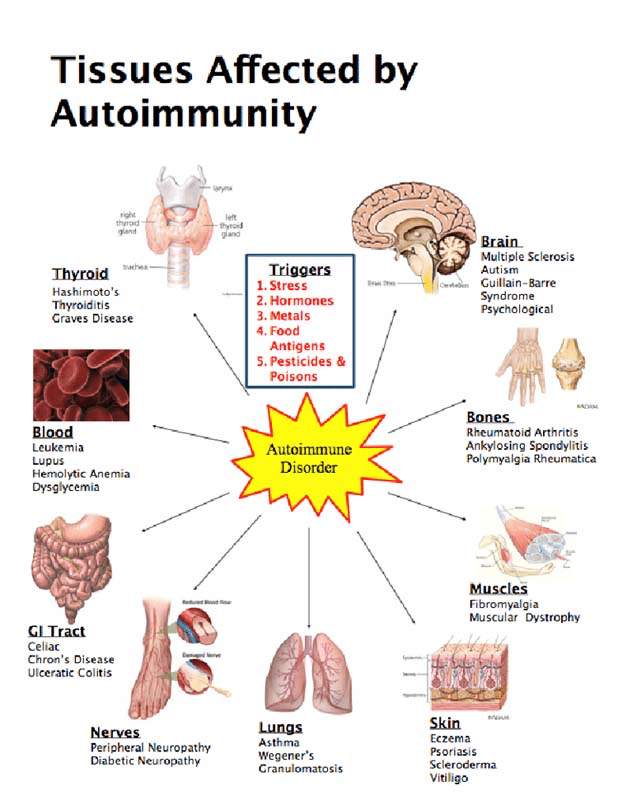
Inflammation and Autoimmune Disease
The truth of the situation is that FOOD MATTERS. That’s right, it’s not just a movie (which by the way you should all watch!). Hyper-permeability of the gut, regardless of whether you can feel it or not is often a significant cause of an extremely long and ever growing list of conditions. The inflammatory cascade that takes place by any inflammatory trigger (diet, medications, infections, stress, hormonal, neurological, or metabolic) can break down the intestinal permeability and allows for the leaky gut mechanism to initiate.
Due to the variety of triggers, it is often possible to reduce an individual’s immune reactivity but not cure it if leaky gut is not the primary trigger for the inflammatory process. There are multiple models of autoimmunity although it is becoming more well accepted that once you develop autoimmunity you will have increased Intestinal Permeability also.
Autoimmunity can be put into remission and this can have profound improved life consequences but it can also be turned on again if life circumstances change. It is considered “Incurable”. You may be able to change the expression of it but to think that you are going to be able to take a boat load of supplements and change your diet and cure the condition you are generally going to be let down.
Waxing and waning responses are par for autoimmunity. When stress picks up despite dietary intake a person will be expected to flare up. This inflammation is initiated by increased levels of iNOS (inducible nitric oxide) which causes an immediate increase in intestinal permeability much like elevated cortisol levels from stress. Once this occurs serum protein particles leak through and become extremely reactive. Gluten is an extremely common serum protein in a situation of increased permeability simply due to the commonality of daily exposure.
If you take on too many projects, eat poorly, have limited or poor sleep patterns, then you can bet that intestinal permeability will increase and food will start to leak through.
Your immune system will then begin to recognize these proteins as other similar proteins like cerebellum, thyroid, etc… When that occurs you will experience symptoms that generally are far removed from what someone would consider to be food related since they are not felt in the gut. Instead you experience brain fog, pain, fatigue, poor sleep, anxiety, or endocrine dysfunction. When antibodies combine with our structural proteins, specific genes are turned on in a special type of immune cell in the body. Inflammatory chemicals are created called cytokines, which are strongly damaging to brain function. In fact, elevated cytokines are seen in such devastating conditions as Alzheimer’s disease, Parkinson’s disease, multiple sclerosis and even autism.
You see, autoimmune disease is not clinically diagnosed until you have tissue destruction. For some neurodegenerative conditions, you need up to 70 percent demyelination (nerve damage) before it will show on an MRI. You cannot afford to wait for that type of advanced destruction before taking action. If you are symptomatic in any way and show to have antibodies or test positive on any of the tests listed above, you have Autoimmune Reactivity and that is enough to take action and make life changes to potentially stop the process from continuing. Inflammation can be a great friend in this sense. Look at it as an early warning sign and take action before it turns into a fire that rages out of control from one body tissue to another.
Recap & Treatment
Inflammation is rampant. In fact 1 in 12 women and 1 in 24 men are dealing with full blown autoimmune mediated inflammation. The number of undiagnosed people is going to be much higher. People with inflammation in the early phases of autoimmunity will often claim no dietary involvement. This is an inaccurate assumption however because the autoimmunity is often triggered by factors not strictly related to diet and the diet can become a secondary trigger later in the development of the condition. If you are dealing with inflammation then get a comprehensive evaluation to look at what is perpetuating your personal fire.
Lifestyle: Remove adverse mechanisms (Stress, Over-exercising, Poor Sleep, Blood Sugar Dysregulation, Poor Social Behaviors.) Lifestyle factors are huge, the stress response triggers immune marker IL6 which turns on the immune pathway TH17 which is the fast track to Autoimmunity.
Lifestyle: Restore beneficial mechanisms: Create conditions of love & appreciation, keep positive attitudes, maintain proper exercise (training to a maximum heart range; i.e. Peak Fitness exercises), have adequate sleep, restore blood sugar balance, and facilitate healthy social interactions. All these things promote natural systemic opioids which pushes the immune pathway TH3 which reduces Autoimmunity.
Dietary Support: Stabilize blood sugar, remove food Autoimmune triggers, and promote intestinal integrity with proper flora and nitric oxide and glutathione pathways. Include fermented foods and supplement appropriately as may be needed.
Remember, a wide array of health problems, including but not limited to chronic pain, obesity, ADD/ADHD, peripheral neuropathy, diabetes, heart disease, stroke, migraines, thyroid issues, dental issues, and cancer are all rooted in inflammation, which must be properly addressed if you wish to be healed.About the Author
Dr. Marquis is a Chiropractic Physician who is Board Certified in Clinical Nutrition in San Luis Obispo County, CA. He also holds certifications in Botanical Medicine, Class IV Laser Therapies, Manipulation Under Anesthesia, Interactive Metronome Therapies and is currently pursuing another Diplomate in Functional Neurology.
David M. Marquis, DC, DACBN
Diplomat American Clinical Board of Nutrition
860 Oak Park Blvd. #202
Arroyo Grande, Ca 93420
(805) 481-3499